How to decide if you might need:
Hysterectomy - removal of the uterus
Oophorectomy - removal of the ovaries
Any surgery should be done for a very good reason, by the most appropriate surgical
route, in the least debilitating way, allowing the speediest recovery of function. Deciding
if the uterus or ovaries should be removed is actually two separate processes, for two
different sets of reasons. So hysterectomy will be considered first and removal of the
ovaries will be discussed later in this paper. First are listed a few definitions, then some
background information about hysterectomy and then a section on all the reasons why
some women would benefit from surgical removal of the uterus while others may
happily avoid surgery.
Total Abdominal Hysterectomy (TAH): This most commonly performed surgery
requires a four to eight inch abdominal incision (vertical if cancer or large mass, and
horizontal for benign and smaller masses) to remove the uterus, and ovaries, if needed.
It can be done for any size uterus, for women who have had children (which relaxes and
loosens the pelvic organ connections and widens the vagina), and those who have not.
There will be a four to eight inch abdominal scar, either sideways or up-and-down, as
required for the specifics of each case. This procedure usually entails two to four days
in the hospital and four to six weeks away from work to recover. This type is still done,
but is the least preferred route by patients because of length of stay, abdominal scar,
pain, and disability. It is sometimes the only route possible, or for women who cannot or
should not have the less invasive techniques listed below.
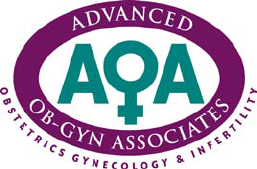
Total Vaginal Hysterectomy (TVH): This is the next most frequent employed technique
of hysterectomy. The surgeon operates entirely through the vagina, pulling the uterus
down through the vagina into view, disconnecting the cervix and then the rest of the
uterus from their internal supports. To use the vaginal route, a woman must not have a
cancer or large mass, and must usually have had a baby or two, which widens the
vagina and relaxes the connections of the uterus so it can be pulled down into the
vagina to do the operation. There is no abdominal scar. It usually requires only two
days in the hospital and about two weeks away from work. Vaginal hysterectomy is a
preferred route if all the specific requirements are met: smallish uterus, no cancer,
vaginal laxity. The only problems with this route is that uterus cannot be significantly
enlarged, the surgeon cannot always get the ovaries out (because they are attached
much higher in the pelvis) when they absolutely need to come out in certain occasions,
cannot examine the upper abdomen, cannot perform it if adhesions are present, cannot
examine for and remove endometriosis, and the patient has a 5-fold higher likelihood of
developing stress urinary incontinence later on.
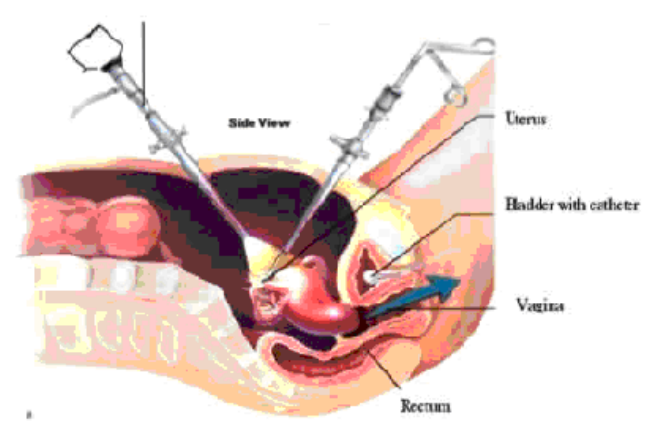
To the Left: Cutaway of
abdomen inflated with gas
to allow surgical removal of
the uterus and ovaries in a
LAVH and TLH.
Laparoscopic Assisted Vaginal Hysterectomy (LAVH): The LAVH also involves
removal of the pelvic organs through the vagina but includes starting with cutting the
ovarian attachments by working through the laparoscopes in the abdomen. It is done
this way because the surgeon thinks that the ovaries probably cannot be disconnected
by operating only through the vagina. LAVH is performed on women who can have a
vaginal hysterectomy but need to be certain the ovaries are removed, or who have had
surgeries which make the vaginal route alone more risky or less successful, or who
have a cancer. There still must be vaginal laxity and openness, as seen after
childbirth. Abdominal scars consist of two to four half-inch incisions. Usually two days in
the hospital are needed with two weeks away from work. Most operating OB/GYN
doctors can do this procedure, but not all. The only problems with this route is that
research tells us that it takes longer and entails a higher blood loss than a total
laparoscopic hysterectomy (see below) and there is still the problem of 5-fold increased
risk of prolapse and urinary incontinence later on.
Laparoscopic Supra-cervical Hysterectomy (LASH): This type of hysterectomy
means that the opening of the uterus was cut from the uterine body and left attached to
the vagina. It is touted as preserving a woman’s sexual function and preventing
prolapse, but research shows that it does neither. Studies comparing women with total
hysterectomy compared to supra-cervical hysterectomy had similar sexual function,
satisfaction and frequency. Research results on many women confirm that there is no
benefit for sexual enjoyment or prevention of urinary incontinence or saggy vagina. The
women with supra-cervical hysterectomies had more monthly bleeding (their periods),
and needed the progesterone supplements in their menopause to prevent hyperplasia
and cancer of the cervix. Many had to have their cervix removed later to alleviate pain
or bleeding that persisted after hysterectomy. A few have developed fibroids,
adenomyosis or cervical carcinoma.
Total Laparoscopic Hysterectomy (TLH): This procedure involves removing the
uterus by operating through the scopes in the abdomen and passing the tissue out
through the vagina or through one of four of the tiny half-inch abdominal incisions.
Large uteri and ovarian cysts, cancer and pre-cancer conditions can all be treated by
laparoscopic hysterectomy. Because there is no operating through the vagina (though
tiny pieces of tissue can be passed down through it), there is no requirement for a wide
vagina or loose ligaments from childbirth, and no problem with increased urinary
incontinence risk later. Hospital stays are shorter and blood loss is about half. Pain is
less and time off from work is only two weeks, not six. There is no increase in risk of
urinary leakage after this type of procedure, and some report that mild leakage was
corrected. This is because your physician connects the inner end of the vagina where
the uterus was attached to the three ligaments that originally held up the uterus (Round
ligament, Uterosacral ligament and Cardinal ligament).
A. In the operating
room
B. These are the
usual incisions for a
laparoscopic
hysterectomy. The
fourth incision is
inside the
bellybutton
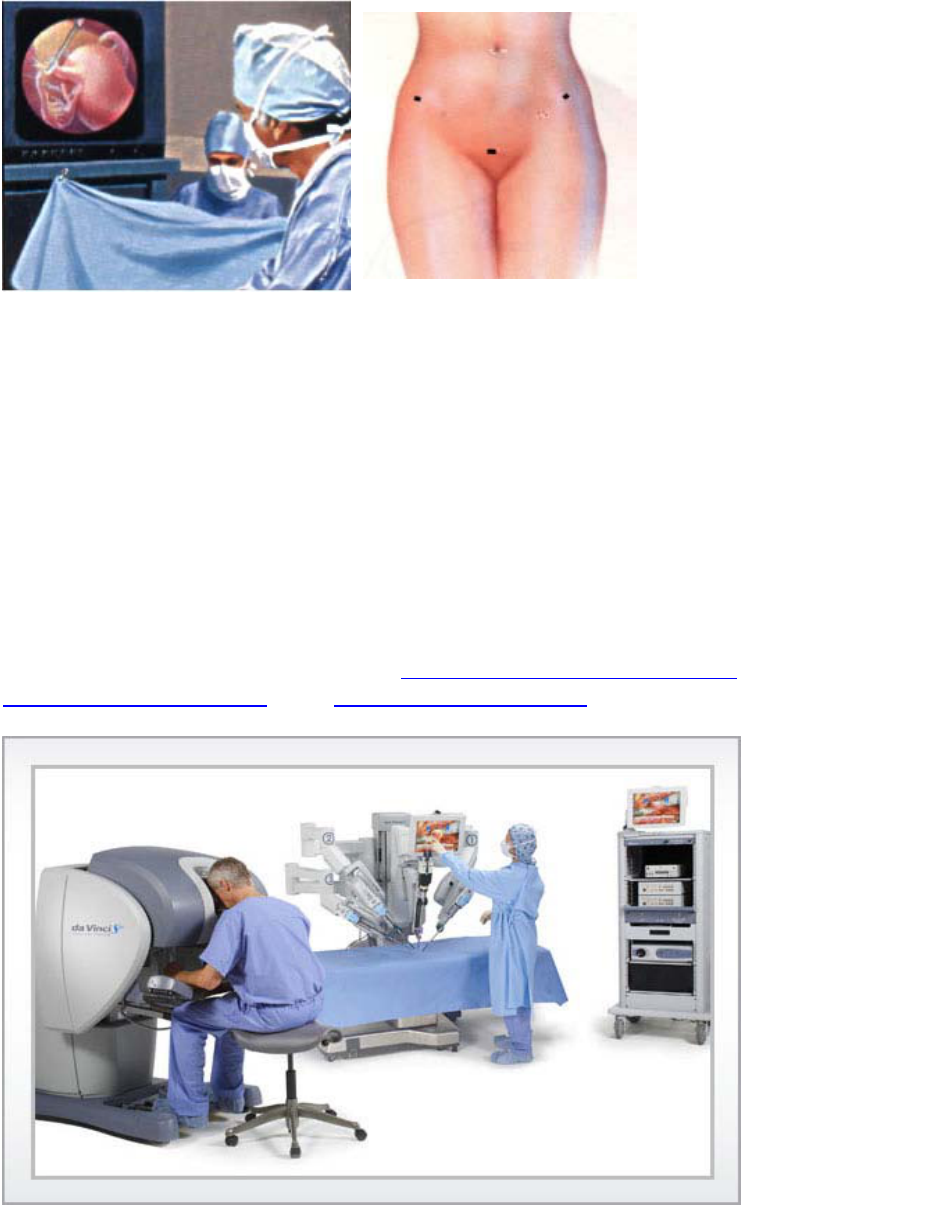
Robotic-Assisted Laparoscopic Hysterectomy: This is the newest form of
laparoscopic hysterectomy. Similar to traditional laparoscopy, small one inch incisions
are made in the abdomen, and the laparoscopic instruments are placed into the pelvis.
The difference between traditional laparoscopic surgery and robotic assisted
laparoscopic surgery is the precision of the robotic instruments. The da Vinci System
provides surgeons with enhanced visualization-including high-definition 3D vision and a
magnified view of the surgical site, increased precision, and better control. While sitting
at the control console, the surgeon controls the system; which translates his or her hand
movements into smaller, more precise movements of the tiny laparoscopic instruments
inside the patient’s body. The blood loss is minimal, the patient has less post-operative
pain, and the patient usually goes home the next day and is back to normal activities in
about two weeks. You can also go to www.daVinciHysterectomy.com ,
www.daVinciStories.com , and www.HysterSisters.com to learn more.
The da Vinci
System:
operating
console on the
left and the
patient console
and patient on
the right.

Now a few facts about hysterectomy: No matter what you have read or found on the
internet, or heard from your friends—what follows are the facts for the vast, vast
majority of women. All the women who had a hysterectomy and are so happy with their
results do not make websites, write books or talk about their surgery, so the internet and
books are not a reliable source for most outcomes. In medicine, we report patients’
opinions and their experiences by analyzing hundreds of questionnaires and publishing
the results so that you know what the probable results of your surgery will be and are
not misinformed or biased by the individual stories that you have heard or read. In
addition, the stories that you have heard or read may have had multiple other factors
that were not accounted for, such as whether or not the ovaries were removed, and if
so, was hormone therapy prescribed afterward? In the correct dose? Why was the
hysterectomy done in the first place? Was it necessary? Was there a cancer? Was
radiation given after the surgery? Were there adhesions? Was there an infection? Was
there endometriosis? All of these factors can impact a woman’s postoperative comfort
and sexual function. So, what follows are the facts.
A. Your Uterus is not a filter: There is a common misperception that there is
a need for women to have a cycle every month to cleanse their bodies. If
that were the case, then what would women who have already had a
hysterectomy use? Or, what would be the analogous male organ and
function? The only true filters your body has are the liver and kidneys, and
to a lesser extent, the lungs and skin. Medically speaking, the only reason
you have a uterus is as an incubator, and the reason you have a cycle
every month is to get the uterus ready for a possible pregnancy next
month. If that is not a desire or concern of yours, then there is no need to
worry about not having a cycle because you have had a hysterectomy.
B. Hysterectomy does not ruin your sex life. Orgasms will be the same.
Lubrication will be the same. Your libido will not change. But be aware that
these things do change as you age, and particularly as a function of your
hormone status. But a hysterectomy is 5 inches away from any of the
nerves of orgasm, and will not ruin any sexual function. Neither will
removal of the cervix with the uterus. If you know someone who claims her
sexual function was worse after hysterectomy, suggest that she see
another gynecologist to make sure that she is hormonally well tuned and
medically well-tuned (thyroid and hormones and other things checked).
From so very many studies, including this 1999 study of 1,299 Maryland
women undergoing hysterectomy, the overwhelming evidence is that
women thrive sexually and emotionally after hysterectomy when the
hormones are tuned and cancer therapy is not needed. In the Baltimore
study, most women had sex more often, and more regularly after their
surgery. 71% had resolution of their previously diminished libido, while
4.3% reported a new problem with low libido after the surgery. 84% had
resolution of pain during intercourse, while 2.3% developed a new pain
during intercourse. 65% of women who had few or no orgasms before
surgery noted improved orgasmic ease and frequency afterwards, while
2.6% developed a new problem with orgasm frequency. After
hysterectomy, more women had stronger orgasm, and fewer women were
sexually inactive. (Rhodes et al, Hysterectomy and sexual functioning,
JAMA, 1999). Your physician won’t operate on you if you don’t stand to
benefit with a strong statistically significantly proven likelihood.
C. Hysterectomy will not cause prolapse of your organs or bladder
leakage. Studies of over 27 thousand women in the Women’s Health
Initiative confirm that hysterectomy does not increase the risk of bladder
leakage, prolapse of the bladder or prolapse of the rectum. (Hendrix,
AJOG, 2002, Hendrix, JAMA, 2005) Having children, smoking and obesity
were the strongest risk factors to predict for incontinence and prolapse In
fact, research also shows that weight loss is one of the most effective non-
surgical remedies for urinary leakage of all types.
D. Hysterectomy will not result in your aging faster. Neither will removal
of the ovaries. If you are under or around age 50, you will probably want to
take hormones for a short while to mimic your natural gradual transition
into menopause. But remember that no matter what, you will continue to
age! (That’s a good thing.) And about 90% of women find they do not
need hormones to feel like their normal selves after their early fifties, even
though most take hormones for until then. The menopausal symptoms
simply go away for most, so the hormones are no longer needed. The
hormones would not and could not prevent aging, wrinkles or arthritis.
E. Hysterectomy will not make you get fat. Neither will removal of the
ovaries. Research tells us that many women gain weight as they age,
especially if they don’t exercise and modify their eating habits. So if you
are going to be one of those women and eat more than you need and
exercise less than you should, then you will gain weight. Hormones won’t
make you gain weight or overeat. In a research project in which women
took a pill for three years, half receiving estrogen and half a placebo or
blank pill, the women on the blank pill gained about 6 pounds and the
women on the estrogen gained half as much. Conclusion: you must
exercise all your life and eat no more than you need all your life.
F. Hysterectomy will not harm your sense of womanhood or femininity.
Some women are afraid that they will no longer be womanly or appear
womanly to their spouses. Nothing could be farther from the truth. Your
sense of womanhood is in your brain, your soul and your heart, but not in
your genitals. No surgery can alter that. If you are under age 50 or so and
have your ovaries removed, you will continue to feel normal with low dose
hormone therapy that mimics your ovarian function until you would have
naturally entered menopause. Please read much more about hormone
therapy in the other brochures. Removing only your uterus creates no
hormonal changes. Your sexual partner cannot specifically tell that you
have had a hysterectomy unless you choose to say so.
G. Hysterectomys should not leave the cervix in place. Research (Thakar
NEJM2003, Kim AAGL2003) comparing outcomes of women who had a
supracervical hysterectomy or total hysterectomy confirm that urinary
frequency, stress incontinence, bowel symptoms, enjoyment of sexuality,
frequency of sexual activity and of orgasm were the same whether the

cervix came out with the uterus or not…but in all reports of supracervical
hysterectomies, up to 25% of women having a sub-total hysterectomy had
cyclical menstrual bleeding and 2% had cervical prolapse (van der Stege,
JSLS,’99) and all of them needed to take a progesterone if they needed
estrogens after their surgery because 23% have estrogen sensitive
endometrium left in (Okaro, BJOG, 2001). There are many reports about
fibroids, chronic pain and cervical cancer in the cervical stump long after
the surgery, necessitating re-operation to remove the cervix in 24%
(Okaro, BJOG, 2001).
Why Would You Need a Hysterectomy?
Removal of the uterus is performed to prevent, alleviate, or treat pain, pressure,
bleeding, or cancer. Each reason is described in detail in the following pages.
1. Cancerous or pre-cancerous problems of the ovaries, uterus or cervix:
Cancer or pre-cancer of the uterus – When cancer grows inside the uterus,
both the womb and the ovaries must be removed in their entirety because they
are lymphatically connected and can allow easy spread to the other organ. The
cervix cannot be left in as any type of uterine or ovarian cancer can spread to the
cervix, making it Stage II rather than I. If a pre-cancer of the uterine lining is
present, it is appropriate in many cases to employ one or two 3-month trials of
progesterones to regress the overgrowth of the lining. This therapy is successful
in about 80% of women who do not have tiny areas of early cancer reported in
their uterine biopsy. If there is still precancerous overgrowth of the lining after two
progesterone trials, then a laparoscopic hysterectomy will be useful in preventing
the progression to a cancer later on.
Pelvic mass, infection, cancer or pre-cancer of the ovaries – A pelvic mass
must be examined by both physician and ultrasonographer to determine if it is a
cancer of the ovary. If the strict criteria for a benign growth are met and no worry
for cancer is present, then no surgery is needed, unless the mass is huge and
imposes by its size or causes pain by twisting. Many women’s ultrasound picture
falls into the gray area of pelvic masses – that is, their ovarian masses have one
or two features of a malignancy, but appear otherwise probably
benign. These
tumors must be surgically investigated by removing them laparoscopically and
giving the tumor tissues to the pathologist to examine under the microscope
during the surgery to see if a malignancy is present. While most are indeed
benign, some are found to be malignant in the earliest stages.
If a cancer is found in an ovary, then the entire uterus and both of the ovaries
must be removed, with the appendix, the lymph nodes and a fatty pad in the
abdomen called the omentum because ovarian cancer likes to spread there. This
is not negotiable, except for one case; unless you have a very rare, early stage of
ovarian cancer that is a very mild type and you have never had any babies, and
plan to. In this rare situation, the ovary can be removed and the cancer staging

procedures done, but the other ovary and the uterus are left in for fertility without
risk to the patient.
Pre-cancer and cancer of the cervix – Recurrent abnormal pap smears which
have been fully investigated by thorough colposcopic (magnified) examination
can often be treated by removal of the uterus. This reduces likelihood that the
pre-cancer will return and reduces chances of either ovarian or uterine cancer. It
is an optional treatment, however, and can sometimes be avoided by careful
colposcopic Laser or Loop treatments, unless so many cervical treatments have
already failed and there is very little cervix left. When cancer of the cervix is
present, a specialized “radical” hysterectomy with a lymph node dissection is
performed through the laparoscopes.
2. Benign problems of the uterus and ovaries, and pain:
Fibroids of the Uterus – Fibroids are round swirls of overgrown benign
muscular fibers in the wall of the uterus. The only reasons to remove a uterus for
fibroid growth are if it causes heavy or chronic bleeding, pain or pressure,
frequent urination, blockage of the ureters (tubes that bring the urine from the
kidneys) or grows during the menopause while not on hormones. Then a total
hysterectomy should be done, usually through the laparoscopes.
But most fibroids DO NOT BOTHER ANYONE!!! The rule is that fibroids that do
not bother anyone should be left alone. Many gynecologists have been too quick
to tell a woman she needs a hysterectomy when her fibroids are not bothering
her, or not bothering her very much. Each woman should be the judge for herself
.
Some women prefer to avoid hysterectomy because menopause is near, and
their symptoms are not too significant. This is reasonable because fibroids
usually shrink about 30% in early menopause. Other women grow fibroids that
are huge or cause discomfort and avoid hysterectomy either because they have
heard awful things about hysterectomies, or they don’t choose to take the time off
from their busy lives to make their life a little more comfortable. Some women
feel they cannot take this amount of time for themselves or draw attention from
their family to have surgery. They should honor their body and value their life
experience and provide for themselves as well as they provide for their families.
Heavy bleeding can be caused by fibroids or polyps on the inner mucous
lining of the uterine cavity either at the wrong times or in huge quantities, even
when the fibroids are small. Uterine polyps, which are small skin tags inside the
cavity, can also cause bleeding, but an ultrasound can show these as separate
from the fibroids. A biopsy will need to be done to confirm that any bleeding is not
due to a cancer in the endometrial cavity. When bleeding is very heavy each
month, many women spend the next few weeks after the period regaining
strength as they use their energy to make new blood to replace the losses. This
cycle, if repeated, or is heavy, can cause anemia, severe fatigue and even
depression this way. A endometrial ablation or laparoscopic hysterectomy can
stop the hemorrhage, prevent anemia, and allow blood stores to replenish,
restoring energy and vitality, and a life free of monthly hemorrhage.

If fertility is desired in a young woman, it is appropriate to remove smaller fibroids
under the uterine lining from a hysteroscopic approach (a scope passed through
the cervix up into the uterus). When fertility is not desired, then the safest,
simplest single approach is to remove the uterus.
Pelvic pain or pressure can be caused by fibroids on the outside of the
uterus. These can become quite large and create a mass effect in your pelvis,
which you can often feel. The larger fibroids can be felt above the pubic bone,
but still may not cause symptoms of pelvic pain, bladder pressure, low back pain
or frequency of urination. When the uterus can be felt below the bellybutton,
many women notice pressure on their bladder or have low back pain.
Laparoscopic hysterectomy is the easiest and safest procedure for them, with
minimal blood loss and maximal probability of resolving the problem with one
procedure.
If a younger woman has large fibroids and realistically desires to preserve her
fertility, it is appropriate to laparoscopically remove the larger outer fibroids. This
should be done about 8 weeks before she desires to becomes pregnant, so the
will not prevent implantation of the pregnancy or cause pain during the
pregnancy. Removal of the fibroids should be done through a horizontal incision,
which is a bigger surgery because the surgeon must cut into the uterus and not
sever any of the major arteries to the uterus. Blood should be donated in
anticipation of this procedure, as the blood loss can be large. Our physicians do
not perform this surgery on peri-menopausal women unless conception is the
clear goal, because it entails taking on major risk for nil benefit except fertility.
Pain in the pelvis can be relieved by hysterectomy with oophorectomy.
Pain before or during periods - Pain can be caused by large fibroids,
endometriosis of the uterus, or adhesions. Endometriosis is the tissue that is
identical to endometrial lining tissue, located in extra-uterine locations. It usually
grows thick and bleeds each month just like the endometrial cavity lining, only it
hurts much more to have this tissue bleeding and sloughing monthly in the wrong
locations. Monthly pain in the pelvis just before and during the period is common
and likely due to endometriosis if it cannot be alleviated by Naprosyn (Alleve).
Always try Naprosyn for gynecologic pain before seeing the doctor, as surgery
can be avoided this way. When Naprosyn does not alleviate the pain, and the
pain is causing a woman to miss work or simply feel awful, she should consider
how long she will keep having the pain without any surgery: usually until
menopause, usually age 51. If this sounds like too long, then consider the
surgery.
When endometriosis is suspected as the cause of monthly pain, then it is
advisable to remove not just the uterus, but also the ovaries, because they can
easily stimulate new growth of endometriosis with the high levels of estrogen that
the ovaries secrete. When the ovaries are left in there is a 50% chance of relief
from pelvic pain. When the ovaries are removed, the relief from pelvic pain is
over 90% likely.
If fertility is desired and endometriosis is suspected based on the pain profile,
then laparoscopic removal of endometriosis is reasonable with conservation of
the ovaries. Preserving the ovaries is essential if fertility is desired, but it also
allows the endometriosis to re-grow over the next year or so, with recurrence of
pain and need for repeat surgery in about 50-75%. This is due to two reasons:
first, the ovaries put out much more estrogen than HRT involves, stimulating re-
growth, and secondly, the ovaries often harbor microscopic or deep nests of
endometriosis that progress and cause more pain or ovarian masses and need
for repeat surgery. Unless fertility is the clear goal, the most effective surgery for
painful periods and pelvic pain in general must include removal of the ovaries.
In addition, the most effective surgery for pain in the pelvis or severe monthly
cramps must involve removal of the uterus. As a woman ages past 40, the
uterine lining can begin grow inside the muscular wall of the uterus
(adenomyosis) and cause pain either all month long or in cycles. This is called
adenomyosis, and it is commonly diagnosed in the mid to late 40’s. This pain
does not respond well to Naprosyn, making endometrial ablation or laparoscopic
hysterectomy/oophorectomy a welcome choice for relief of pain.
Pain during sex. Painful sexual activity involving deep thrusting into the vagina
is usually caused by endometriosis, adenomyosis or, possibly adhesions from a
prior surgery. If Naprosyn doesn’t relieve pain during sexual activity, then an
anatomic cause is suspected and surgery can relieve this pain with reasonable
effectiveness.
Infection of the uterus, tubes or ovaries. Because pelvic infections are
frequently recurrent and occasionally associated with malignant changes,
surgery to remove the uterus, tubes and ovaries is standard, especially if fertility
is completed.
Quality of life: do you deserve it? Hysterectomy causes short-term morbidity,
but appears to increase average life expectancy slightly among peri-menopausal
women and is cost-saving. Medical outcomes and economic consequences favor
the hysterectomy over trying to preserve the uterus as medical remedies are
most often unsuccessful, and ultimately the surgery needs to be done. Research
on women undergoing hysterectomy shows that 78% are symptom free after
their operation, and another 14% have reduced symptoms, while 8% have new
symptoms. Fully 95% report that they were pleased with their HRT or it exceeded
expectations, 5% reported not liking their HRT because for some it contained
testosterone. Physical well-being was improved in 80% and unchanged in 15%
and worse in 4.6%. 32% noted less depression than before the surgery, while
65% had no depression, and 4% became more depressed. Overall, 3% were
dissatisfied. Satisfaction was associated with understanding the need for the
surgery, a positive outlook, removal of the ovaries, taking HRT for at least the
short-term, complete symptom relief, a quick recovery, improved physical well-
being, and the absence of depression. (Khastgir et al, Am J Ob/Gyn, 2000) In
another study, at 12 and 24 months after their hysterectomy 95.8% and 96.0%,
respectively, reported that the hysterectomy had completely or mostly resolved
the problems or symptoms they had before surgery; 93.3% and 93.7%,
respectively, reported that the results were better than or about what they
expected; 85.3% and 81. 6%, respectively, reported that their health was better
than before the hysterectomy; and 87.9% and 93.1%, respectively, reported
being totally recovered.
After reviewing your symptoms that have led you to review this document, it is
only you who can decide whether you life could be significantly improved by
eliminating the gynecologic problems that brought you to this point. If your
problems do not impact the quality of your life, then there is no benefit to surgery.
If you have significant room for improvement, then make the decision to create a
new life for yourself. You definitely deserve it.
Hysterectomy FAQs (Frequently Asked Questions)
Will I be happy after I have a hysterectomy?
The highest probability is that you will forget that you had a hysterectomy
because your uterus will no longer be a source of pain or pressure or bleeding or
cancer. Because we only do hysterectomies on women who, based on medical
evidence, will benefit from them; our patients are healthier after their surgery than
they were before. Ask any of them.
How safe is having a hysterectomy?
A hysterectomy is a major surgery, and all surgeries have risks associated with
them. Your doctor will discuss the risks, benefits, and alternative options with you
prior to your surgery. Different surgical indications and individual patient’s
circumstances and preferences direct surgeons to prefer one hysterectomy over
another. Rest assured, your surgeon will offer the hysterectomy that gives you
the best chance to achieve the best results for you, with the least risks, and the
quickest recovery.
How much pain will I have after the hysterectomy?
There will be some discomfort when you wake up from surgery, less with
laparoscopic hysterectomies and the traditional open abdominal hysterectomies.
Some measures are taken during the surgery and before you wake up to
minimize the discomfort, and medicine will be given in recovery and during your
hospital stay to minimize your discomfort. You will be given a prescription for
medication when you leave the hospital to take while you are home. If you need
additional refills, please call our office and let us know and we will be happy to
call in a refill for you.
How long will the procedure take?
Depending on the type of hysterectomy and the reason for the hysterectomy,
along with any unforeseen problems, can contribute to the length of your surgery.
If you are having a robotic procedure, it usually takes a little longer to get
everything in it’s proper place once you have been put to sleep. Tell your family
members and support team to expect about 2 ½ hours, but your doctor will let
you and them know specifically when you are seen prior to your surgery.
What happens after the surgery?
Usually, you can expect to go home the next day after surgery, however if your
doctor thinks or you feel you need to stay an additional day, most insurances will
pay for the additional day. When you get home, you are encouraged to begin
walking the next day. Nothing strenuous, just causal walking. You can begin
driving at one week from your surgery. By two weeks, you should be able to
resume your normal activities. Unless you have a strenuous job, you can return
to work if you like. By four weeks, you should be able to do anything you like,
except for intercourse (see below).
How soon can I have intercourse after my hysterectomy?
With traditional hysterectomies, you can usually resume vaginal intercourse after
4 weeks. With robotic-assisted hysterectomies, you will need to wait 10 weeks to
resume vaginal intercourse. The reason is the way the vagina is opened to
remove the uterus and the way it is closed. It takes longer to heal using robotic
instrumentation. It is a small price to pay for you (your husband/partner might
disagree) for the quicker recovery. If you have vaginal intercourse too soon, you
risk the end of your vagina tearing open and potentially your intestines coming
partially out of your vagina. We have seen it happen! Other forms of intimacy are
fine, just nothing in the vagina until 10 weeks.
How long will I need to be off work?
If you do not have a physically strenuous job, you can potentially return after 2
weeks from a robotic hysterectomy, 4 weeks after a traditional hysterectomy.
You can take off up to 4 weeks without a note from your doctor. More than 4
weeks will require a medical reason and your doctor will have to exam you to
determine if additional recovery time is needed. We will be happy to fill out your
short term disability and/or FMLA. It usually can be completed in 7-10 business
days and will cost $50.
If my doctor recommends a robotic-assisted hysterectomy, will
my insurance cover the procedure?
We always your call your insurance to recertify your procedure. While the
insurance industry, in general, will not guarantee payment for any procedure prior
to the procedure; we have not had any problems with coverage for the
procedure. We will not do any procedures without contacting your insurance
company and doing everything in our power to assure coverage and payment.
How do I schedule my procedure?
All you need to do is call the office and select the prompt to schedule your
procedure. Once you instruct us to schedule your procedure, we will take care of
the rest for you. We ask you to call us 3-4 week before you want your surgery to
give us time to contact your insurance to recertify your surgery If you have time
constraints, please make us aware of these and we will do our best to schedule
your procedure at your convenience.
Conclusions
Many women choose to keep their gynecologic symptoms because the
symptoms are not bothersome, but those few women disabled by significant
symptoms can have great improvement in their lives with surgery. When the
reasons are real and strong for a hysterectomy and/or removal of the ovaries,
women usually emerge from the surgery and recover their normal whole-life
function with ease and vigor. We don’t fix what ain’t broken, so no one will have a
hysterectomy/oophorectomy unless she really stands to benefit from one! Always
be certain that you agree with all the reasons for any surgery proposed, and that
all your questions have been thoroughly answered. Do not go to any surgery
unless you are convinced of the need for it, aware of the benefits, have run out of
non-surgical alternatives, and understand all the risks. If your doctor doesn’t
answer all your questions, hire another doctor
Why Would You Elect to Remove the Ovaries?
Removal of one or both of your tubes and ovaries (unilateral or bilateral salpingo-
oophorectomy) can be performed at the same time as your hysterectomy; or if needed,
at a later date. However, there is no need to remove the tubes and ovaries at the same
time of your hysterectomy, unless there is a problem. Listed below are different reasons
to keep your tubes and ovaries, and reasons to have them removed.
If you are still involved in your fertility years, an ovary should be removed only if
there is a large, complex or persistent mass on it or if you have intolerable pain from
endometriosis. There should be an attempt to preserve the portion of the ovary that is
normal, and to make sure the other ovary is also normal. While relief from your pain is
not guaranteed, and cysts or tumors may recur, surgery is effective in making certain
that there is no cancer, and can reduce or eliminate the pain temporarily for conception.
However the pain or mass may re-develop in the future whenever the ovaries and
uterus are left in for fertility purposes.
If you are past your fertility years and need surgery for a mass or for pain and
have normal ovaries, then consideration should be focused on permanent relief of
pain, reduction in need for further surgery, preventing ovary and reducing risk for breast
cancer.
If a woman undergoing hysterectomy is over 50 and has no problems with her
ovaries, no pain suggestive of endometriosis or adenomyosis and no family history of
breast or ovarian cancer, she should still consider having the ovaries removed
incidental to her hysterectomy. It is recommended only because the risk of ovarian
cancer in her lifetime is about 1.7% with a 1.5% chance of dying of it. Among the risk
factors for ovarian cancer are increasing age, obesity, prior breast cancer,
endometriosis, prior infertility treatments, never having had a baby, and a family history
of ovary or breast cancer. In one study of women who developed ovarian cancer, 14%
of the women had previously had a hysterectomy and had preserved their ovaries.
While it is impossible to say that all 14% could have prevented their ovarian cancer by
having the ovaries removed earlier, it is reasonable to assume that most cases would
have been prevented by removal of the ovaries.
Removing the ovaries will put you into menopause but the hormone therapy to keep
you feeling normal is now done well and will keep you feeling normal. The goal would
be for you to take bio-identical estrogen in a lower dose than your ovaries released, but
enough to keep you feeling yourself, tapering the dose so you enter a natural
menopause at about age 51 when most women enter menopause. Normally, the
ovaries cease function at about age 51, with no known functional benefit after that age,
only risk. This is why the Standard of Care is to recommend removal of ovaries incident
to hysterectomy for women over age 45. This is the softest reason for removing the
ovaries. This reason is should be a very individualized decision for each woman. Ask for
the information brochure on hormones for women around their menopause.
Estrogen replacement therapy until age 51 or so can be done easily and safely, and
simply eases a woman into the same transition that she will enter into during the next
few years of her life. In fact, replacement therapy doses of pure estrogen are much
lower than the levels normally made daily up to age 51 by the ovaries. These low doses
of pill, ring or patch estrogens are lower than the levels that the ovaries naturally
secrete, and can easily prevent hot flashes, and protect bone density without any
increased risk of heart disease or breast cancer, until age 60, according to the Women’s
Health Initiative reports. There is a lifelong decrease in new and recurrent breast cancer
risk after removal of the ovaries, even if women take low doses of pure estrogen to
prevent hot flashes. It is entirely safe for women to use estrogen after their
hysterectomy/oophorectomy until the age that the ovaries naturally quit, 51; and safe for
even ten more years, the Women’s Health Initiative tells us. Heart disease and breast
cancer risk were actually slightly lower for women using estrogen alone between ages
50 and 60.
Pelvic mass is not cancer: Your ovaries should be removed if there is a mass
greater than 6 cm, or a cyst of any size that has solid parts, or if there is a significant
chance that a benign cyst can recur at a later date (e.g., endometriosis) requiring repeat
surgery. If you have completed your fertility, eliminating pain, avoiding further surgery,
and preventing a cancer become the priorities. If there is a complex overgrowth of
tissue replacing the bulk of your ovary, then it should be removed to rule out the
possibility of cancer. Ultrasound or sonography (same) is used by both the abdominal
view--a wand is moved over the skin of your abdomen, and the vaginal view--a small
wand is placed inside your vagina-- to obtain precise measurements of the ovaries and
the uterus. This is the best tool for examining the pelvic organs.
Relieve significant pain, during menses, during sex or other activity which can
result from tumor growth, adhesions or endometriosis. Leaving even a normal
appearing ovary inside when treating endometriosis or pelvic pain reduces the chance
of successful pain relief from over 90% to under 50%. This is because the normal ovary
secretes high levels of estrogen and can re-stimulate growth of endometriosis in the
pelvic organs, and because the ovary itself is a popular site for endometriosis to grow at
any time, even if it looks normal to the surgeon during surgery. For this reason it is
advisable to remove both ovaries for greatest success in relief, if pelvic pain is the
reason for surgery.
Relieve disability from premenstrual symptoms (PMS) including premenstrual
migraines and mood disorders such as severe anxiety, rage, and depression. Very few
women have such severe symptoms that their lives are seriously impacted, but for
some, these symptoms can be quite disruptive to their orderly living, PMS emotional
changes can make some women do things they regret, or have to undo or apologize for
out of control behavior, scheduling vacations and important events to avoid their
episodes of PMS. Other symptoms such as depression, over-eating, lethargy, rage,
tender breasts, migraines, etc. during the 3-10 days before your period starts may
simply be bothersome. When birth control pills and antidepressants have not caused
relief, removal of the ovaries is necessary, and providing pure estrogen in even daily
doses. This can restore a woman to her even, normal, best function. For those few
women with this degree of symptoms, removal of the ovaries can be life-restoring.
Prevention of hormone-related migraines, which typically occur just after ovulation,
and just before the menstrual flow, can be accomplished by removal of the ovaries. This
stops estrogen fluctuations completely and reduces or eliminates the cycle-related
migraines. Both the uterus and ovaries must be removed, however, to obviate the need
to balance any estrogen with progesterones which can cause PMS symptoms. After the
removal of both ovaries and uterus, one only needs to take estrogen alone, which is the
hormone that dominates during the second week of the cycle, when women feel most
normal, even, and free of migraines.
To prevent ovarian cancer. If a woman is not from a family with a known high-risk for
ovarian cancer, her risk is about 2% and reduced down to zero by ovary removal, Given
the high mortality rate (80%) of ovarian cancer, primary prevention strategies for ovarian
cancer should be used whenever possible. From another research report: by removing
women’s ovaries who are having surgery and past their fertility, the overall incidence of
ovary cancer would decrease by 15%, breast cancer rates would decrease by 50%, and
colon cancer rates would decrease by 15% (Cape, Eur J Cancer Prev 1999). Research
shows that few women undergoing prophylactic oophorectomy have regret about their
decision.
To prevent ovarian cancer in women from families with cancers of the breast,
ovary, colon, stomach, lung, and lymphomas. The risk of ovarian cancer was
increased 50% in women with a family history of cancer of the stomach, 70% with
intestinal cancer, 30% with lung cancer, and more than 200% with breast cancer or
lymphomas.(Negri, et al. Eur J Cancer, 2003) Risk of ovary cancer is 17-fold, or nearly
10% lifetime risk, when the family history is positive for relatives with ovarian
cancer.(Burgfeldt et al, Lancet, 2002) The chance of developing ovarian cancer
associated with a family history of breast cancer was 2-10 times that of women not
reporting a family history of breast cancer.
To prevent ovary and breast cancer in women with hereditary cancer genes.
Among women who have a gene mutation for inherited breast and ovarian cancer (BrCa
1, 2, or HNPCC) removing the ovaries reduces ovarian cancer risk from about 27-44%
to about 2-3%.(Rebbeck et al, NEJM, 2002)
Such women need annual rectovaginal pelvic examination, testing of CA 125 level, and
transvaginal ultrasonography until completion of fertility. Oral contraceptive use appears
to reduce the risk of ovarian cancer while fertility is being conserved. Once fertility is no
longer needed, prophylactic oophorectomy/hysterectomy is suggested.
Women found to have a genetically increased risk of breast cancer should be counseled
about options for management, including close surveillance, lifestyle modifications,
chemoprevention with tamoxifen, enrollment in a breast cancer prevention clinical trial,
and prophylactic mastectomy and/or oophorectomy.
To reduce risk of new breast cancer in the general population. Having the ovaries
removed, especially early before menopause, reduces risk of new breast cancer by
50%, a benefit which lasts a lifetime. This may be because ovulations with progesterone
secretion are eliminated, or because subsequent estrogen levels are lower, even with
ERT.
To reduce breast cancer recurrence in women with prior breast cancer. Survival
from breast cancer is improved, and the risk of ovarian cancer is greatly reduced
by oophorectomy. Oophorectomy reduces new same-sided and opposite-sided breast
cancer and recurrent breast cancer. The risk of new breast cancer was reduced in
women who underwent bilateral oophorectomy with hysterectomy by 30-50%. The
protection tended to increase with time since surgery, (Schairer et al, Int J Cancer,
1997, and Parazzini et al, Obstet Gynecol, 1997). The risks of subsequent breast
cancer from low-dose ERT are not elevated over normal. It is shown that prophylactic
oophorectomy may have a substantial protective effect on breast cancer risk despite
subsequent low-dose or non-low-dose ERT, especially when prophylactic
oophorectomy is performed at an early age.
Quality of life: do you deserve it? Hysterectomy causes short-term morbidity, but
appears to increase average life expectancy slightly among perimenopausal women
and is cost-saving. Medical outcomes and economic consequences favor the
procedure. Research on women undergoing hysterectomy shows that 78% are
symptom free after their operation, and another 14% have reduced symptoms, while 8%
have new symptoms. Fully 95% report that they were pleased with their HRT or it
exceeded expectations, 5% reported not liking their HRT because for some it contained
testosterone. Physical well-being was improved in 80% and unchanged in 15% and
worse in 4.6%. 32% noted less depression than before the surgery, while 65% had no
depression, and 4% became more depressed. Overall, 3% were dissatisfied.
Satisfaction was associated with understanding the need for the surgery, a positive
outlook, removal of the ovaries, taking HRT for at least the short-term, complete
symptom relief, a quick recovery, improved physical well-being, and the absence of
depression. (Khastgir et al, Am J Ob/Gyn, 2000)
After reviewing your symptoms that have led you to review this document, it is only you
who can decide whether you life could be significantly improved by eliminating the
gynecologic problems that brought you to this point. If your problems do not impact the
quality of your life, then there is no benefit to surgery. If you have significant room for
improvement, then make the decision to create a new life for yourself. You definitely
deserve it.
Will I be happy after I have a hysterectomy/oophorectomy?
The highest probability is that you will forget that you had this surgery because your
uterus/ovaries will no longer be a source of pain or pressure or bleeding or cancer.
Because we only do hysterectomies on women who, based on medical evidence, will
benefit from that surgery; our patients are healthier and happier after their surgery than
they were before. Ask them.
Conclusions. Many women choose to keep their gynecologic symptoms because the
symptoms are not bothersome, but those few women disabled by significant symptoms
can have great improvement in their lives with surgery. When the reasons are real and
strong for a hysterectomy and/or removal of the ovaries, women usually emerge from
the surgery and recover their normal whole-life function with ease and vigor. We don’t
fix “what ain’t broke”, so no one will have a hysterectomy/oophorectomy by our
physicians unless she really stands to benefit from one! Always be certain that you
agree with all the reasons for any surgery proposed, and that all your questions have
been thoroughly answered. Do not go to any surgery unless you are convinced of the
need for it, aware of the benefits, have run out of non-surgical alternatives, and
understand all the risks. If your doctor doesn’t answer all your questions, hire another
doctor!
